I tell the truth right up front—I turned to mounjaro injection weight loss when my usual tricks stopped working. I was juggling dinner, dishes, and a dancing toddler. I felt worn out, worried about my blood sugar, and out of simple options.
I talked to my doctor first. I asked hard questions and read clear, reliable information. Then I decided to use the drug as one tool in a plan. It wasn’t a magic fix. It was a weekly routine that fit real life—grocery day, soccer practice, and sanity checks.
I worried about side effects, cost, and time. I made a plan, took notes, and kept my care team in the loop. Over weeks I noticed steady changes—less constant cravings, more energy, and small wins at the dinner table.
Key Takeaways
- I chose this option after talking with my doctor and reading trusted information.
- It helped with appetite and blood sugar, but it’s not a quick fix.
- Expect steady progress over time, not overnight results.
- Common effects include GI symptoms; discuss risks and follow-up with your doctor.
- This guide shares real routines, simple food tips, and questions to bring to your visit.
Cozy Kitchen Confession: Why I Looked at Mounjaro Injection Weight Loss in the First Place
That midnight fridge light moment pushed me to pick up the phone and call my doctor. I was tired of guessing. I kept seeing the same patterns on labels and in my days.
So here’s how I do it: I wrote down my top questions first—safety, realistic timelines, appetite changes, and how a new drug might fit a busy week. I asked about type and diabetes risks, too.
The night I read labels by fridge light and decided to call my doctor
I remembered small, honest details—snacks after bedtime, energy dips, and how clothes felt. I noted the problem without shame. That list made the visit focused and useful.
Future-facing hope: setting realistic goals in a “new meds” world
My goals were kitchen-first: steadier blood sugar swings, steady energy, and simple meals I could make with a toddler on my hip. I set limits—no perfect days, just better choices more often.
- I tracked progress beyond the scale: how clothes fit and how long I stayed full.
- I set tiny rituals: a pen by the calendar and a fixed day each week for notes.
- I told my family what dinners might look like and why this mattered for long-term health.
Many people feel hopeful but hesitant about a new drug. I did too. So I started small, kept my care team close, and promised myself honest notes for the next appointment.
What Is Mounjaro, Really? GLP-1 + GIP in Plain English
Let me explain the science without the lab coat—just simple, real talk. This medicine acts like a two-button system in your body. It helps calm hunger and steady blood sugar so daily meals feel easier to manage.
Dual agonist 101: glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide
Tirzepatide hits two targets: glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide (GIP). Think of each as a tiny messenger that tells your body to release insulin after a meal and to slow the stomach a bit.
Why two receptors may mean stronger appetite control and steadier blood sugar
Both messengers work together. That combo can give stronger effects on fullness and post-meal glucose. For me, meals felt satisfying sooner and afternoons were calmer.
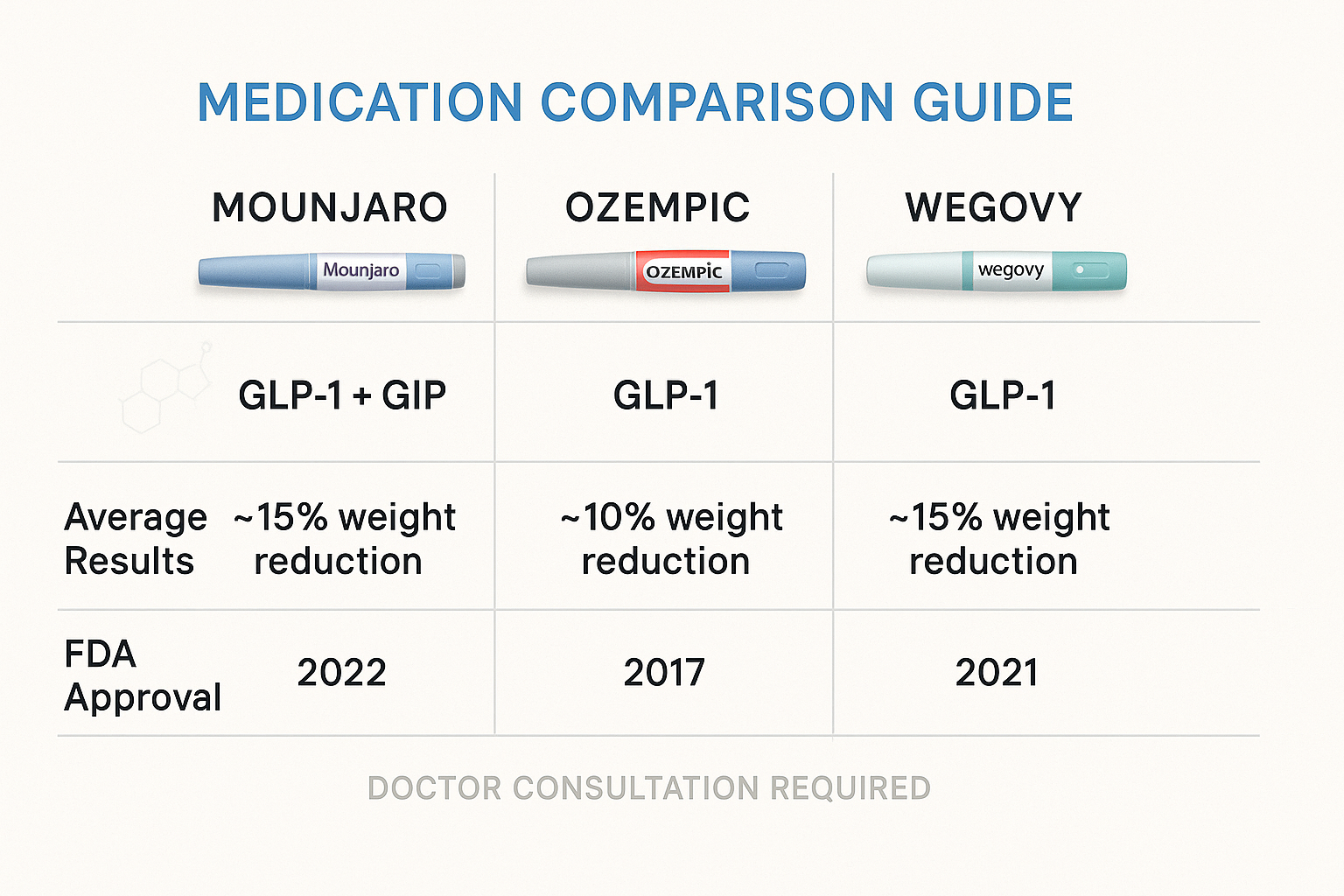
How it differs from semaglutide drugs like Ozempic and Wegovy
Semaglutide mainly taps GLP-1. This drug taps GLP-1 and GIP. Studies in people with type 2 diabetes showed greater average weight changes with the two-button approach. Still, use always needs a doctor’s plan.

“It felt like swapping a big plate for a smaller one—without the hunger.”
Is Mounjaro Approved for Weight Loss, or Is It Off-Label?
The approval story matters, so I dug into labels, insurance rules, and what my doctor would actually prescribe.
Quick fact: This drug is FDA-approved for type 2 diabetes. It is not labeled for reducing weight in people—that makes using it for that goal an off-label approach.
The now vs. the near future: off-label use and fast-moving approvals
Meanwhile, Zepbound (same active ingredient, tirzepatide) has an approved label for adults with obesity or overweight plus a related condition.
That difference matters. Off-label use can affect insurance coverage, pharmacy stock, and out-of-pocket costs. Talk to your doctor about which option fits you and how coverage might change.
Zepbound explained: same tirzepatide, different label
- Ask your doctor which product and dose to start—many clinicians begin at 2.5 mg weekly and step up every four weeks.
- Report any lumps, hoarseness, or trouble swallowing—these are symptoms tied to a boxed warning from animal studies about thyroid cancer risk.
- Bring prescription details to appointments and plan follow-ups for sugar goals and side checks.
| Feature | Mounjaro | Zepbound | Practical note |
|---|---|---|---|
| FDA approval | type 2 diabetes | weight management (adults) | Labels differ; coverage varies |
| Active ingredient | tirzepatide | tirzepatide | Same molecule, different label |
| Typical start | 2.5 mg weekly | 2.5 mg weekly | Dose increases every ~4 weeks |
| Coverage likelihood | more likely for diabetes | may qualify for adults with obesity | Check insurer policies |
“Confirm the label, discuss dose, watch symptoms, and plan follow-ups with your doctor.”
Mounjaro Injection Weight Loss: What the Studies Say About Results
When I read the trial numbers, I turned those percentages into jeans and forks. SURMOUNT-1 showed adults without diabetes lost a lot over 72 weeks—higher doses reached roughly 20% body change. That looks like a smaller plate at dinner and a looser waistband on a favorite pair of jeans.
Average change and what it feels like
In practical terms, a 10% shift can mean going down a size or feeling less snack-driven after lunch. People with type 2 diabetes on tirzepatide saw bigger body changes than many on semaglutide in head-to-head data.
Why stopping can mean regain
Trials that paused treatment around 36 weeks often saw some return over time. Continuing through 88 weeks helped maintain or deepen results. Time and consistent dosing matter—most studies titrated every four weeks.
“I felt fullness sooner, but the stomach stuff hit early when my dose climbed—so start slow.”
Common side effects were GI issues, so many patients and doctors choose slower steps to ease the side on the way up. My doctor watched blood pressure and blood work and adjusted the plan as I reported real-life problems like travel or missed doses.
For a clear medical summary, see this trusted explainer and bring your prescription questions to your doctor.
How It Feels Week by Week: My First Months on a Once-a-Week Pen
The first week felt like learning a new kitchen rhythm—small adjustments, big signals.
I started low: 2.5 mg for four weeks, then my provider and I stepped up every four weeks as tolerated. That steady dose plan kept surprises small.
Starting low and stepping up
I picked one day and one time each week. That tiny ritual made the weeks predictable. If a day went off—travel or a party—I restarted the next week and kept going.
Noticing fullness sooner
Meals changed first. I felt full faster, so I served less and ate slower. Tiny bites, long pauses—my stomach calmed and the afternoon sugar cravings eased.
- I logged the effects each week—sleep, energy, bathroom notes—and texted a quick update to my doctor.
- Mild nausea showed up when I increased dose; ginger tea and bland meals helped.
- Simple prep—rotisserie chicken, canned beans—made weeknights easy and kept routine doable.
“Small, steady changes beat dramatic ones—my body liked that pace.”
| Week range | Common feelings | Practical tip |
|---|---|---|
| Weeks 1–4 | Mild hunger change, routine building | Pick a day/time and prep simple proteins |
| Weeks 5–12 | More fullness, brief nausea with increases | Slow bites, ginger tea, note symptoms for your doctor |
| Ongoing | Steadier appetite and calmer sugar swings | Keep a short log and be gentle with missed weeks |
For a practical read on early adjustments, see this your first month guide.
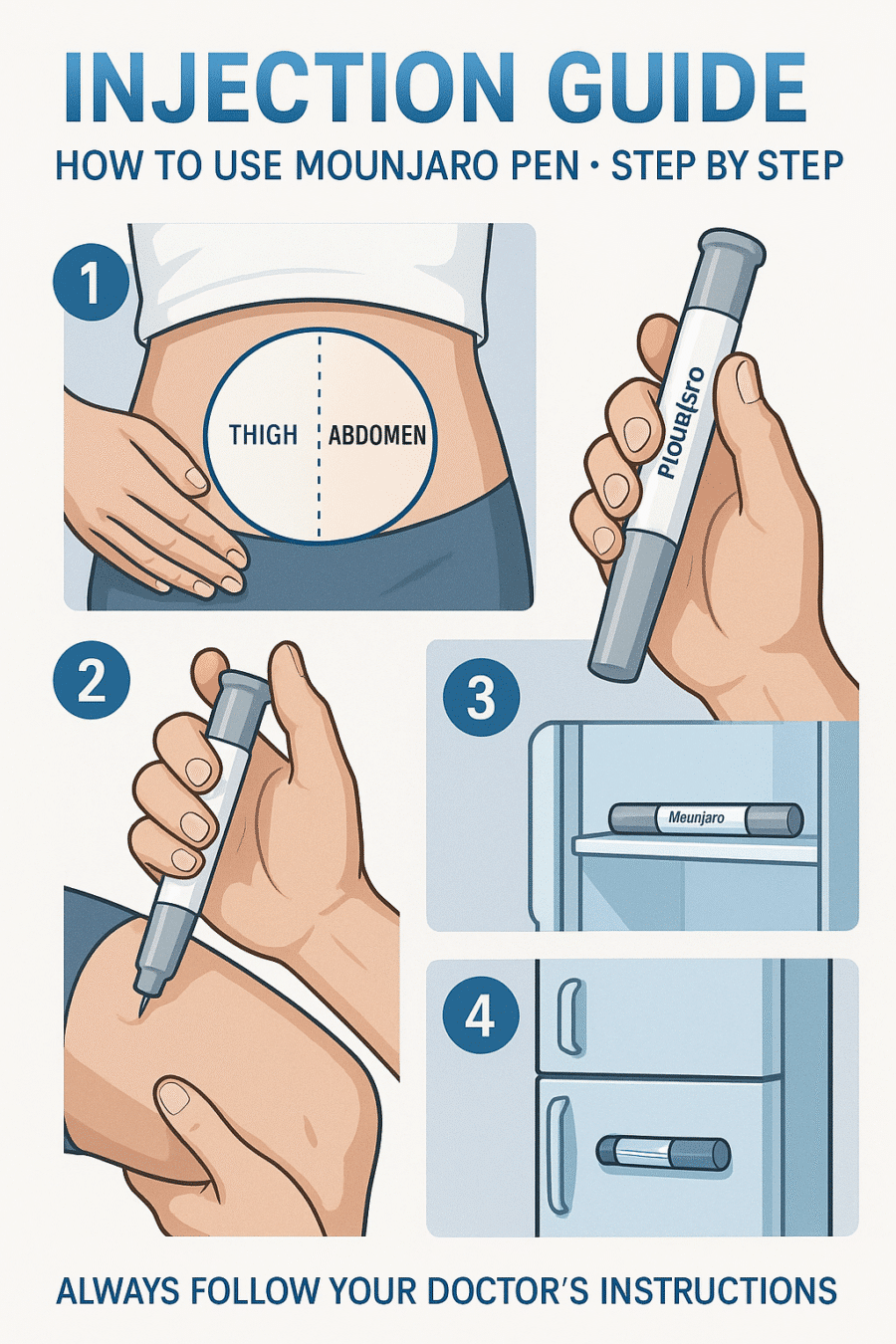
How to Use the Pen: Where to Inject, When, and Tiny Tricks That Help
A single small habit—same day, same time—kept me from missing a week. I picked Sundays and made the pen part of my morning routine. That tiny rule made it feel doable.
Best sites and skin care
Where: I inject subcutaneously into the thigh or abdomen. A caregiver can do the upper arm.
I rotate sites each week. I skip bruised or scarred skin. That helps avoid irritation and keeps routines painless.
Simple step-by-step routine
- I check the pen and the dose window first.
- I clean the spot, pinch gently, inject, then count slowly before pulling the needle out.
- I take a deep breath to steady my hand—works every time.
- I stash the pen with vitamins and set a phone reminder so use becomes automatic.
- I log sites and any tiny blood spotting in a notebook to spot trends.
- I message my doctor if unusual redness, pain, or swelling appears.
“A calm, repeatable rhythm turned a medical task into a quick, no-drama habit.”
I prep a small protein snack after. It helps if I feel shaky. For a clear guide to using the pen, check this link—it’s practical for patients starting the drug and avoiding common problems and side checks related to blood or skin.
Dose, Timing, and Titration: Building a Plan With Your Doctor
I sat down with my doctor and we sketched a clear plan—low start, slow steps. We agreed on goals that mattered to me: calmer sugar swings, more energy, and steady changes in weight.
Common starting dose and safe step-ups for adults
We began at 2.5 mg once weekly for four weeks. Then we planned to raise by 2.5 mg every four weeks, up to 15 mg, only if I felt okay.
- I tracked how each dose felt—nausea, fullness, sleep, and energy.
- My doctor and I treated increases like test drives: pause if side effects rose.
- I kept my prescription notes current so the clinic always knew my status.
When to pause, when to hold steady, and when to advance
If nausea spiked or appetite dipped too hard, we paused. Holding steady helped many patients adjust without giving up progress.
- Pick one time of day for a shot to avoid missed doses—set a second reminder as backup.
- Plan breaks for travel or holidays with your doctor so the plan fits real life.
- Ask for labs on a set schedule so you and your clinician see the full picture.
“Start low, step slow, and keep your care team in the loop.”
Side Effects I Watched For (And What My Doctor Flagged)
I kept a small warning list from day one—things my doctor wanted me to watch for closely. I stayed calm, but I tracked every new feeling so I could act fast if needed.
Common GI issues I looked for were nausea, vomiting, diarrhea, and constipation. Small meals, slower bites, and ginger tea helped me. I also rotated sites when a spot looked sore.
Serious problems to report
- Sudden, severe belly pain or persistent vomiting — could be pancreatitis.
- Signs of low blood sugar if you have diabetes or use other meds — shakiness, sweating, confusion.
- Dehydration that stresses the kidney — keep water handy and sip often.
Boxed warning and who should avoid it
There’s an animal-based boxed warning about thyroid cancer. If you or close family have medullary thyroid cancer (MTC) or MEN2, this drug is not for you. Watch for a neck lump, hoarseness, or trouble swallowing and call your doctor right away.
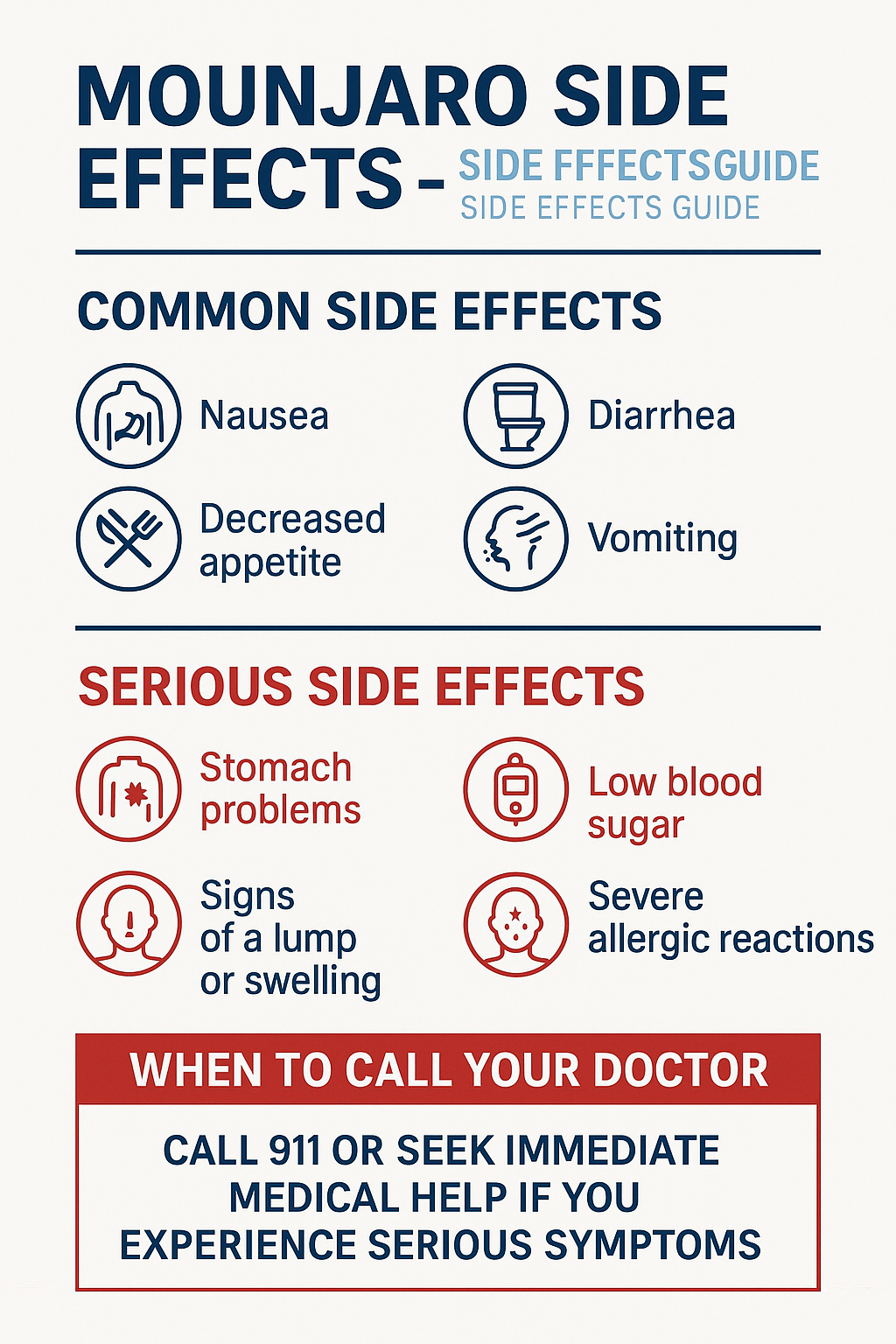
“Track symptoms, hydrate, and call if pain is severe or new signs appear.”
Quick plan: note side effects, rest the stomach, sip fluids, rotate injection spots, and contact your care team for red flags. That steady routine kept me safe and sane.
Food, Fullness, and Blood Sugar: Eating So You Feel Human
Food became my safety net—the simple kind that keeps me steady on tough days. I learned to pair small plates with a plan so my appetite felt manageable and my blood sugar stayed calmer.
Why high-fat meals can make symptoms louder
Higher-fat dishes slow stomach emptying. That extra slowing plus a dose-change week can make nausea and other side effects louder.
So I avoid heavy sauces and deep-fried meals when my body feels sensitive. It helps reduce queasy moments and other problems.
Small, protein-forward meals that sit well
I favor tiny, protein-rich bites—eggs, tender chicken, beans, yogurt. They fill me up without overfilling my stomach.
Simple carbs—oats, rice, fruit—round meals out and keep energy steady. I stop at the first sign of fullness. No drama, just saving the rest for later.
Quick wins and kitchen hacks
- Sip ginger or peppermint tea when nausea nudges in.
- Pack easy snacks: string cheese, nuts, or cottage cheese with fruit.
- Make a short “feel-good” list so dinner doesn’t become a guess.
- This one’s saved my week more than once: quick mug recipes at BusyCookLife.com.
“Gentle food, smaller portions, and kindness to yourself go a long way.”
| Issue | Foods to Favor | Foods to Avoid |
|---|---|---|
| Nausea or queasiness | Ginger tea, plain yogurt, toast | Fried foods, heavy cream sauces |
| Low appetite | Small protein bites, smoothies with protein | Large, fatty entrees |
| Blood sugar dips | Oats, fruit, balanced snacks | Large sugary treats |
Comparing Meds: Mounjaro vs. Ozempic, Wegovy, and Zepbound
When I stacked the drugs on paper, the differences felt less like right vs wrong and more like trade-offs. I want to be practical—mechanism, results, and how my body handled the change mattered most to me.
Mechanism, effectiveness, and tolerability
Semaglutide targets glucagon-like peptide-1. It helps slow appetite and steady blood sugar. Tirzepatide taps GLP-1 and GIP, so it may blunt hunger more and affect glucose a bit differently.
In trials for people with type 2 diabetes, tirzepatide showed larger average changes in body size than semaglutide. Both drugs share similar GI side effects—nausea, diarrhea—but how severe they are varies by person.
Why “better” depends on you
Think about goals, coverage, and daily life. Some pick a drug for stronger appetite control. Others choose cost or an approved label for treating health conditions.
“Pick the tool that helps you meet blood sugar goals, tolerates well, and fits your budget.”
| Feature | Semaglutide (Ozempic/Wegovy) | Tirzepatide (Zepbound / Mounjaro) |
|---|---|---|
| Target | GLP-1 | GLP-1 + GIP |
| Average body change in diabetes trials | Moderate | Higher on average |
| Common effects | GI symptoms; dose ramping | GI symptoms; often steeper early effect |
Check labels, ask about the right dose, and confirm prescription coverage before you commit. Your body and your insurer will help decide which drug fits your life.

Money, Access, and Insurance: The Not-So-Fun Part
Money talks—and this part of the journey had more paperwork than my taxes. I learned fast: off-label use often means bigger bills, while a labeled product can unlock coverage for some people.
Off-label costs, coupons, and why pharmacies run short
Off-label fills may be denied by insurers. Coupons sometimes exclude off-label use. Pharmacies face limits and rerouting during shortages. I called early, asked about stock, and avoided last-minute trips.
Talking to insurers and doctors about coverage pathways
Bring clear information to calls: diagnoses, BMI, prior attempts, current prescription, and your doctor‘s notes. Ask about prior authorization and step therapy before you start.
- Script to try: “Hi, I need coverage info for this drug. My doctor prescribed it for medical reasons. What documentation do you need?”
- Ask your clinic about samples, manufacturer programs, or telehealth plans that help patients bridge access gaps.
- Watch common problems: coupon exclusions, refill limits, and pharmacy allocation during shortages.
“Keep tidy paperwork, set reminders for authorizations, and follow up weekly until it’s solved.”
I also told my provider about past kidney issues and family history. That matters—boxed warnings like thyroid cancer in animals show why you must report symptoms fast.
Get written info from your doctor so you can compare options calmly at home. Advocate for yourself—clear questions, tidy paperwork, and steady follow-ups make a real difference.
Who Should Consider It—and Who Should Not
Before you decide, here’s a plain-spoken look at who often benefits and when to pause. I talked this through with my doctor, and we checked family history and labs first.
Adults with obesity or overweight plus conditions: candidacy basics
Some adults qualify under the Zepbound label: BMI ≥30, or ≥27 with related conditions like hypertension, dyslipidemia, or sleep apnea. These patients may be considered when lifestyle steps alone aren’t enough.
- Ask your doctor if your medical profile and goals fit the plan.
- Think about your whole body history—past meds and side effects matter.
- Bring a full med list and recent labs so the team sees the full picture.
When to press pause: pregnancy, MEN2/MTC risk, kidney or eye problems
Pause if you’re pregnant, trying to conceive, or breastfeeding. Stop and talk to your doctor first.
- A personal or family history of MEN2 or medullary thyroid cancer means this is not for you — that risk is real.
- Use caution with recent pancreatitis, severe GI disease (like gastroparesis), diabetic retinopathy, or reduced kidney function.
- Check for interactions with other medication and plan around surgery or procedures.
If you have type diabetes or prediabetes, monitoring changes in sugars and eye health is key. Share any new symptoms quickly.
“Pick a path with your doctor that fits your risks, your life, and your hopes.”
Conclusion
Here’s the short, honest wrap-up I wish someone had handed me at the start.
I kept one rule: team up with my doctor and take small steps over time. Medication is a tool, not a shortcut. Pair it with simple meals, steady sleep, and gentle movement for the best chance to lose weight and keep it off.
Track what you notice—good effects, any side effects, and quick checks of blood work when your clinician asks. Plan refills and authorizations early so access doesn’t break your rhythm.
Watch for new neck lumps or unusual signs tied to thyroid or rare cancer warnings and call your doctor fast. Be patient. Be kind. You can lose weight and feel human doing it—one calm choice at a time. Thanks for cooking and learning with me.
FAQ
What is tirzepatide and how does it work?
Tirzepatide is a prescription drug that acts on two gut hormones — glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). I think of it like a two-pronged signal that helps curb appetite and improves blood sugar control by slowing stomach emptying, reducing hunger, and helping insulin work better when glucose is high.
Is this drug the same as semaglutide (Ozempic, Wegovy)?
Not exactly. Semaglutide targets GLP-1 only. Tirzepatide hits both GLP-1 and GIP receptors. That dual action often means stronger appetite suppression and different effects on blood sugar, but individual responses and side effects can vary.
Is tirzepatide FDA-approved for treating obesity?
As of now, tirzepatide (sold under different brand names for diabetes and weight) has approvals that depend on the labeled indication. Some formulations are FDA-approved for type 2 diabetes, while an associated brand, Zepbound, carries specific approval for chronic weight management. Off-label prescribing still happens — talk to your doctor about options and risks.
What kind of weight change did clinical trials show?
In trials, many adults saw significant reductions over months, often more than older incretin drugs. Results vary by dose, lifestyle changes, and how long people stayed on therapy. Stopping the drug can lead to weight regain, so long-term planning with your clinician matters.
How do people usually feel week to week after starting a once‑weekly pen?
Early weeks often bring mild to moderate GI symptoms — nausea, some vomiting or diarrhea, maybe constipation. I found appetite changed first; I felt full faster and smaller meals worked. Most side effects eased with gradual dose increases and time.
What are the common side effects I should expect?
The most common are gastrointestinal — nausea, vomiting, diarrhea, constipation, and sometimes decreased appetite. These are usually dose-related and often get better after a few weeks. Staying hydrated and eating small, protein-rich meals helps.
Are there serious risks I need to know about?
Rare but serious issues include pancreatitis, gallbladder problems, severe low blood sugar (especially if combined with insulin or sulfonylureas), and a boxed warning about thyroid C‑cell tumors in rodents. People with personal or family history of medullary thyroid carcinoma (MTC) or MEN2 should avoid it. Always discuss your medical history with your provider.
How is blood sugar affected, and who needs closer monitoring?
Tirzepatide generally lowers blood sugar in people with type 2 diabetes — that’s one reason it’s used. If you take insulin or sulfonylureas, your doctor may lower those doses to prevent hypoglycemia. People with kidney disease or advanced diabetic eye disease need careful follow-up.
How do you use the pen and where do you inject?
It’s a once‑weekly subcutaneous pen. Common sites are the thigh, abdomen, or upper arm — rotate spots each week. Your healthcare team will show you proper technique, storage, and how to pick a consistent day to make it stick in your routine.
What’s the usual dosing plan and titration schedule?
Many start at a low dose and increase every 4 weeks until a maintenance dose is reached, to reduce side effects. Exact dosing depends on the brand and indication. Your prescriber will set the plan based on your goals, tolerance, and medical history.
Can I take this if I’m pregnant or planning to get pregnant?
No — it’s not recommended in pregnancy. If you’re planning pregnancy or become pregnant, stop the medication and talk to your clinician about alternatives and safe management of weight and blood sugar.
How should I eat while on this medication?
Many people do better with smaller, protein-rich meals and fewer high‑fat or greasy foods, which can worsen GI symptoms. Slow bites, chew well, and keep snacks handy for low blood sugar if you’re on other diabetes meds.
What about drug shortages and cost — will insurance cover it?
Coverage varies. Diabetes indications are more likely to be covered than off-label weight use. There can be copay programs, manufacturer savings, or prior‑authorization hoops. Pharmacies may have intermittent supply issues, so plan ahead with your provider and insurer.
Who is a good candidate, and who should avoid it?
Adults with type 2 diabetes or adults with obesity/overweight plus related conditions may be candidates. Avoid if you have personal/family history of MTC or MEN2, pregnancy, or certain severe GI or pancreatitis histories. Kidney or eye disease requires extra caution — check with your doctor.
How long do you need to stay on it to keep results?
Maintenance often means ongoing treatment. Stopping usually brings gradual return of appetite and possible weight gain. Long-term plans should include lifestyle support and regular medical follow-up to decide what’s right for you.
What symptoms require immediate medical attention?
Severe abdominal pain (could signal pancreatitis), persistent vomiting or dehydration, signs of severe hypoglycemia (confusion, fainting, seizures), or sudden vision changes need urgent care. Call your provider or emergency services right away.
Can this medication affect my thyroid or increase cancer risk?
Animal studies showed thyroid C‑cell tumors, which led to a boxed warning. Human risk is unclear but cautious approach is standard. People with a history of medullary thyroid carcinoma or MEN2 should not use it. Discuss personal risk with your clinician.
How do I talk to my doctor about starting this medication?
Be honest about goals, medical history, and daily routine. Ask about dosing, side effects, monitoring plans, costs, and how it fits with any other meds. I found writing questions down before the visit really helped keep the chat focused.