I’m Emma — 37, living in Asheville, a mom who cooks from the heart between toddler naps. I started this path because my blood sugar needed steady help and my weight felt stubborn. I chose a realistic route that fit family meals, messy counters, and weekend hikes.
This is honest. I’ll tell you what worked, what flopped, and how I kept cooking simple while tracking my blood numbers. I learned that tiny habits move the needle more than dramatic fixes.
I read studies, talked with clinicians, and used trusted resources like the Cleveland Clinic to learn about tirzepatide — see the overview here. I also watched my sugar trends and asked about risks, including rare thyroid concerns.
Expect short tips, plain talk about safety, and real kitchen-life hacks. I’ll share how I remembered doses, handled nausea days, and kept my home cozy while chasing better health.
Key Takeaways
- My story shows practical ways to use a prescribed treatment safely in daily life.
- Small, steady changes helped blood readings and eased daily routines.
- Talk to a clinician about risks like thyroid issues before you start.
- Simple meal swaps kept flavor and routine without extra stress.
- Tracking trends beats guessing — but don’t let numbers rule your day.
Why I Chose This Path: A Cozy, Real-Life Introduction to mounjaro for diabetes and weight loss
That Tuesday night, after the last dish hit the sink, I finally said yes to a new plan. I needed something that fit messy mornings, toddler naps, and real meals. I wanted steady blood numbers and tiny wins that lasted.
The night I said “okay, let’s try it”
I said yes on a Tuesday—sticky plates, a sleepy kid, and one deep breath. I didn’t want a dramatic overhaul. I wanted small habits that stuck in my week.
The focus keyword in my daily life: mounjaro for diabetes and weight loss, four ways it showed up
That phrase kept showing up—in my notes, in clinic questions, in grocery lists. It became a practical idea, not just a headline.
- Simple routines: I picked one calm time each week to check numbers.
- Tiny habits: Microwave breakfasts and visible pens made tracking easy.
- Slow titration: Most people start low and increase after a week or so—this helped my stomach adjust.
- Support: I texted a friend on rough days and asked clear questions at visits.
What I needed most at the start: simple steps, honest expectations, steady support
So here’s how I do it: I stacked tiny habits, tracked one number at a time, and celebrated small wins. The first shifts were small—less post-meal spike and easier porch climbs—but they mattered.
“Patient routines worked like good stock simmering low and slow.”
I wrote a short list of bland, cozy foods that calmed my stomach. I made peace with slow change. That steady, human approach kept me going.
What Mounjaro Is (and Isn’t): Plain-English Basics Before You Start
My goal was simple: clearer mornings and fewer sugar swings without upending family life. I wanted straight facts about the medicine so I could decide with my clinician.
FDA status and real-world use
Big picture: This drug (tirzepatide) is FDA-approved to treat type 2 diabetes. A sibling brand, Zepbound, is approved weight loss in adults with obesity or related conditions. Clinicians may prescribe tirzepatide off-label to help with weight loss. Off-label use can affect insurance coverage.
How it works in the body
It mimics two gut hormones—GIP and GLP-1. GIP nudges more insulin after meals. GLP-1 slows stomach emptying and curbs appetite. Together they lower glucose swings and steady blood sugar.
- Once-weekly subcutaneous injection via pen or vial.
- Typical start at 2.5 mg weekly, then slow increases to find the right dosage.
- Clinical trials showed meaningful HbA1c and fasting sugar drops and notable weight changes at higher doses.
| Feature | What to expect | Notes |
|---|---|---|
| Mechanism | GIP + GLP-1 agonism | Boosts insulin after meals; slows gastric emptying |
| Format | Weekly injection | Single-use pen or vial |
| Clinical impact | Lower A1C and fasting glucose | Also shows meaningful changes in weight over time |
| Access | Approved to treat type diabetes | Off-label use may need clinician judgement and billing checks |
I tracked meals and symptoms. That simple log gave my clinician useful information when we adjusted my dose. If you want more practical notes on how I used it, see my step-by-step guide at use mounjaro.
Safety First: Boxed Warnings, Red Flags, and When to Call the Doctor
Before anything else, I learned the clear warning signs to watch for. Safety mattered more than any quick win. I kept notes and asked my clinician about every new symptom.
Thyroid tumor risk and who should avoid it
Important: There’s a boxed warning about thyroid C-cell tumors. If you or close family have medullary thyroid carcinoma (MTC) or MEN2, this drug is not an option. Watch for a new neck lump, a persistent hoarse voice, or trouble swallowing—call your clinician right away.
Pancreas, gallbladder, kidney, and vision concerns
Pancreatitis can start suddenly. Severe upper belly pain that shoots to your back, plus vomiting, is an emergency—stop using the drug and call right away.
Gallbladder problems can show as sharp pain, fever, or yellowing skin. Dehydration from GI effects can strain kidneys—sip fluids and check urine output.
Quick changes in blood sugar can affect vision. Report any blurring or loss of sight to your eye doctor and clinician.
Allergies, mood, and urgent steps
Serious allergic signs—swelling of face or throat, trouble breathing—need emergency care right away. Mood shifts or suicidal thoughts also need fast contact with a clinician or support person.
- Rule I follow: when in doubt, act. Your health comes first.
- Travel with medical ID and keep prescriptions handy.
- For practical dosing notes, see my mounjaro dosage guide.
| Risk | Watch For | Action | Urgency |
|---|---|---|---|
| Thyroid C-cell tumor | Neck lump, hoarseness, trouble swallowing | Stop and call clinician | Right away |
| Pancreatitis | Severe upper belly pain, back pain, vomiting | Stop drug; seek medical care | Right away |
| Gallbladder disease | Sharp pain, fever, jaundice | See clinician or ER | Right away |
| Allergic reaction / Mood changes | Swelling, breathing trouble, suicidal thoughts | Emergency services or clinician contact | Right away |
So Here’s How I Do It: Dosing, Titration, and That Once-a-Week Rhythm
I started slow and kept a simple rhythm so my stomach and schedule could adapt. I began at 2.5 mg once weekly for four weeks. That gave my body time to settle and let me watch how meals felt.
Typical start and gradual increases
After the first month, we raised the dose by 2.5 mg every four weeks as tolerated — 5 mg, 7.5 mg, 10 mg, and up to 15 mg if needed.
This slow plan kept nausea low and my week predictable. I tracked sugar after meals and sent notes to my clinician before each change.
Practical rhythm & safety checks
- I picked one calm day of the week and one time of day to inject. Repetition stuck better than apps.
- If I had to shift a dose, I kept at least 72 hours between doses.
- Because I used other meds, we watched for low blood sugar. My clinician adjusted insulin when A1C was near target.
- I never stopped on my own — stopping can raise blood sugar and bring back weight quickly.
“Small, steady changes won my week — and my stomach — back.”
Want a practical dosing checklist? See my detailed dosage guide to pair with your plan.
Shots Don’t Have to Be Scary: Injection How-To You Can Actually Use
Holding that tiny device felt strange at first, but practice made it normal fast. I kept things simple and steady. Short steps, calm hands, and a plan helped me build confidence.
Pen or vial: what goes where and how to rotate spots
I used the single-use prefilled pen. It’s quick and tidy. I pick the abdomen, thigh, or upper arm and rotate each week so my skin stays happy.
Rotate like a clock: upper right, upper left, thigh, belly. That keeps absorption even and lowers irritation.
Timing, missed doses, and keeping your routine realistic
I set a phone reminder for the same day of the week. If life forces a switch, I wait at least 72 hours before the next dose.
Missed a shot? I check the instructions and call the pharmacist. They helped me keep my schedule steady and my blood sugar tracking useful.
Travel tips, storage basics, and avoiding counterfeit pens
Travel with a cooler pouch, your prescription, and a note with dosing day and time. Plan across time zones so meals and doses line up.
Store the pen per label—no freezing, no hot trunks. Single-use means one and done; sharps container only. Buy from reputable pharmacies. If packaging looks off, call Lilly Answers Center at 800-545-5979.
“Little routine, big confidence—the more I practiced, the less I thought about the needle.”
| Topic | Quick tip | Why it matters | Action |
|---|---|---|---|
| Injection site | Rotate abdomen, thigh, arm | Even absorption, less irritation | Switch spot each week |
| Timing | Same day each week | Builds routine, helps tracking | Set phone reminder |
| Missed dose | Wait ≥72 hours if changing day | Avoids overlap or gaps | Call pharmacist if unsure |
| Storage & safety | Follow label; use sharps container | Preserves drug and safety | Pack cooler for travel; verify pharmacy |
Making Meals Work for You: Keeping Blood Sugar Steady Without Stress
I learned to treat meals like tiny safety nets for shaky days. Small, steady bites helped my body adjust when GI changes hit. Simple shifts cut nausea and kept sugar from swinging wildly.
Small, frequent, gentle meals to ease nausea and prevent lows
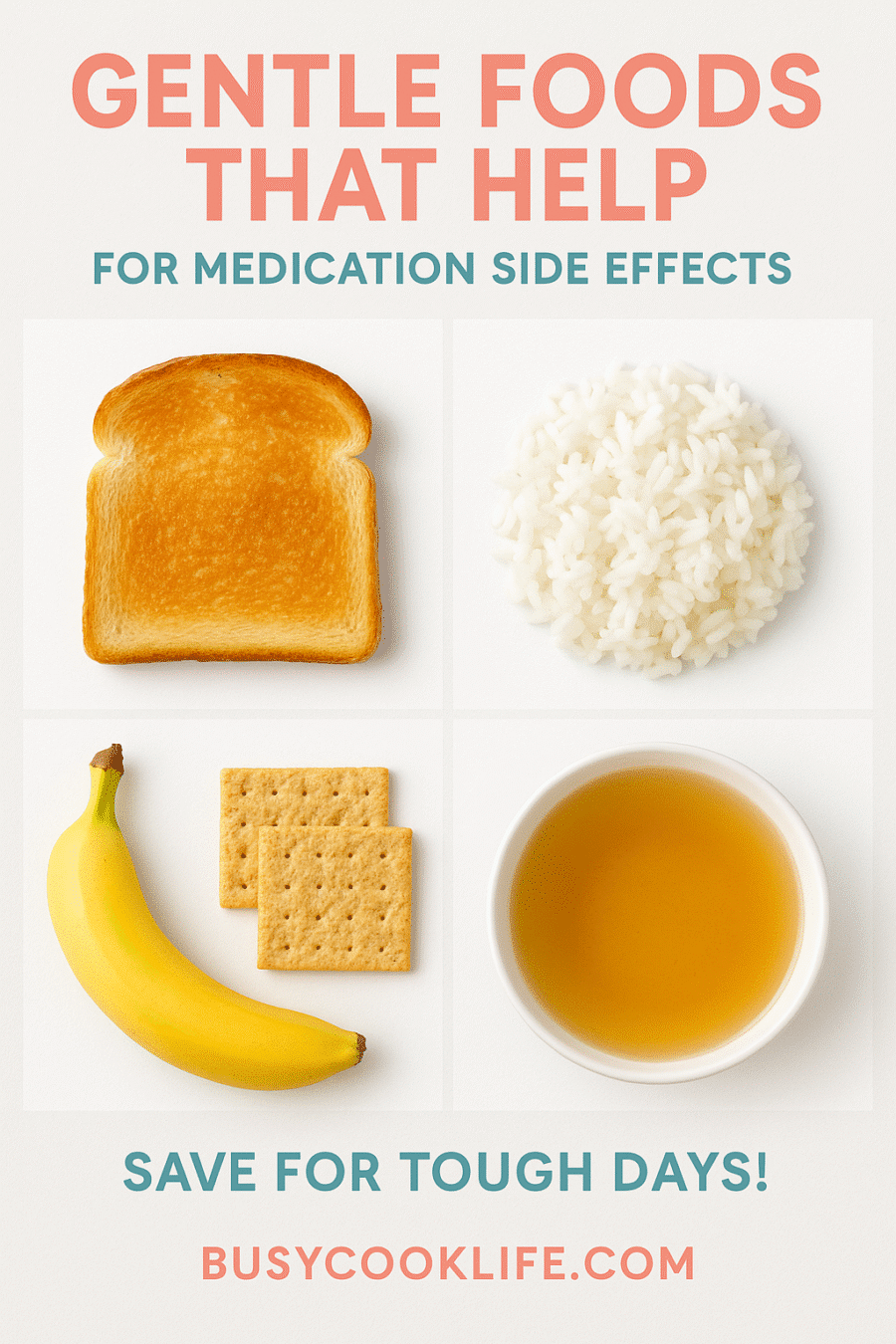
Eat little and often. Tiny meals kept my stomach calm and helped me avoid dips when I used insulin or sulfonylureas. Bland choices—toast, rice, crackers, banana—worked best on rough mornings.
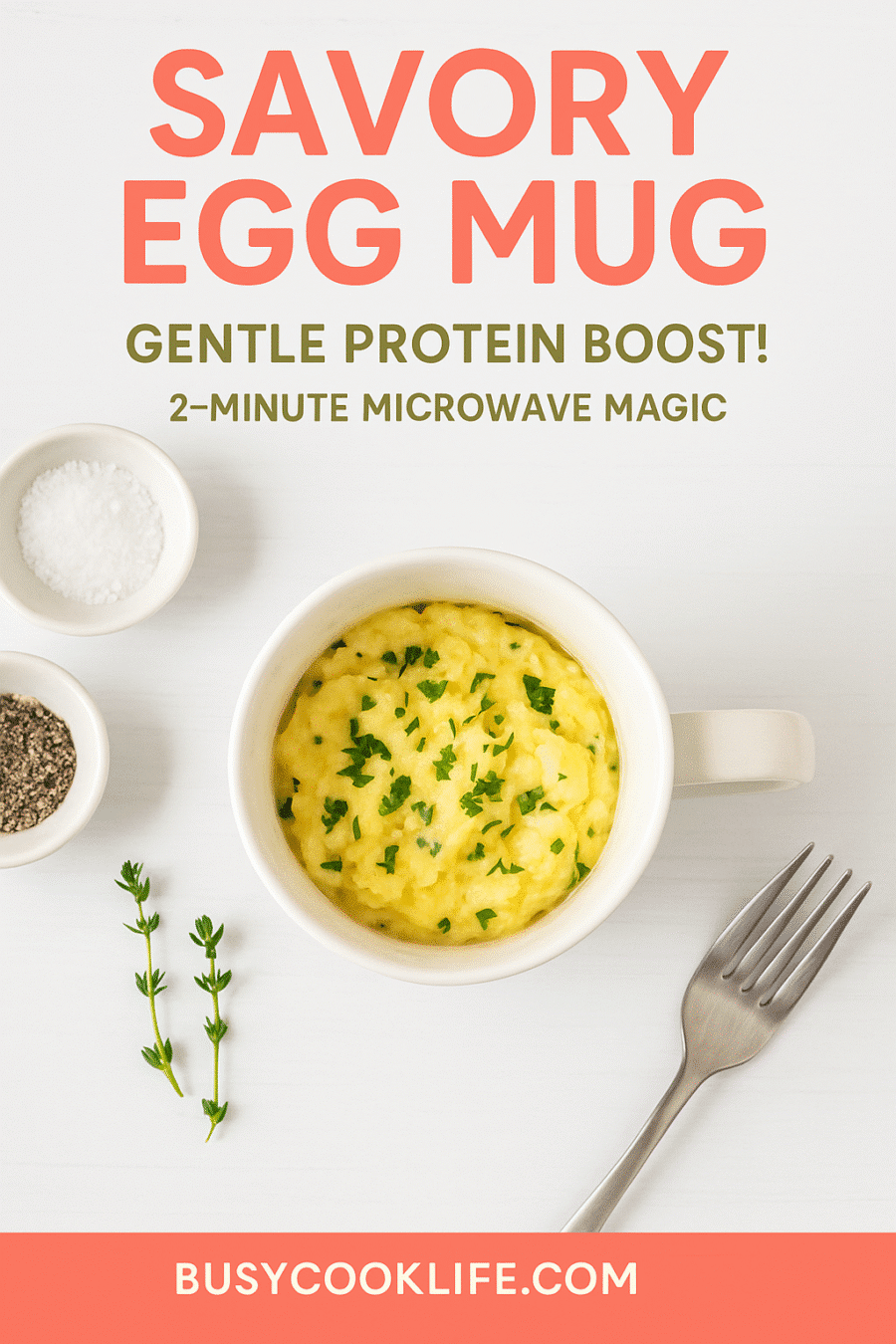
I balance protein and carbs. An egg or Greek yogurt with toast holds me longer than carbs alone. When nausea flares, I lower the fat for a day or two.
Hydration habits that support your body’s GI adjustment
Sip clear liquids all day. Broth, herbal tea, or water with a pinch of salt helps prevent dehydration. If vomiting happens, stick to clear fluids and call your clinician if you can’t keep liquids down.
Easy microwave helpers: BusyCookLife.com Cozy Mug Oats and Savory Egg Mug
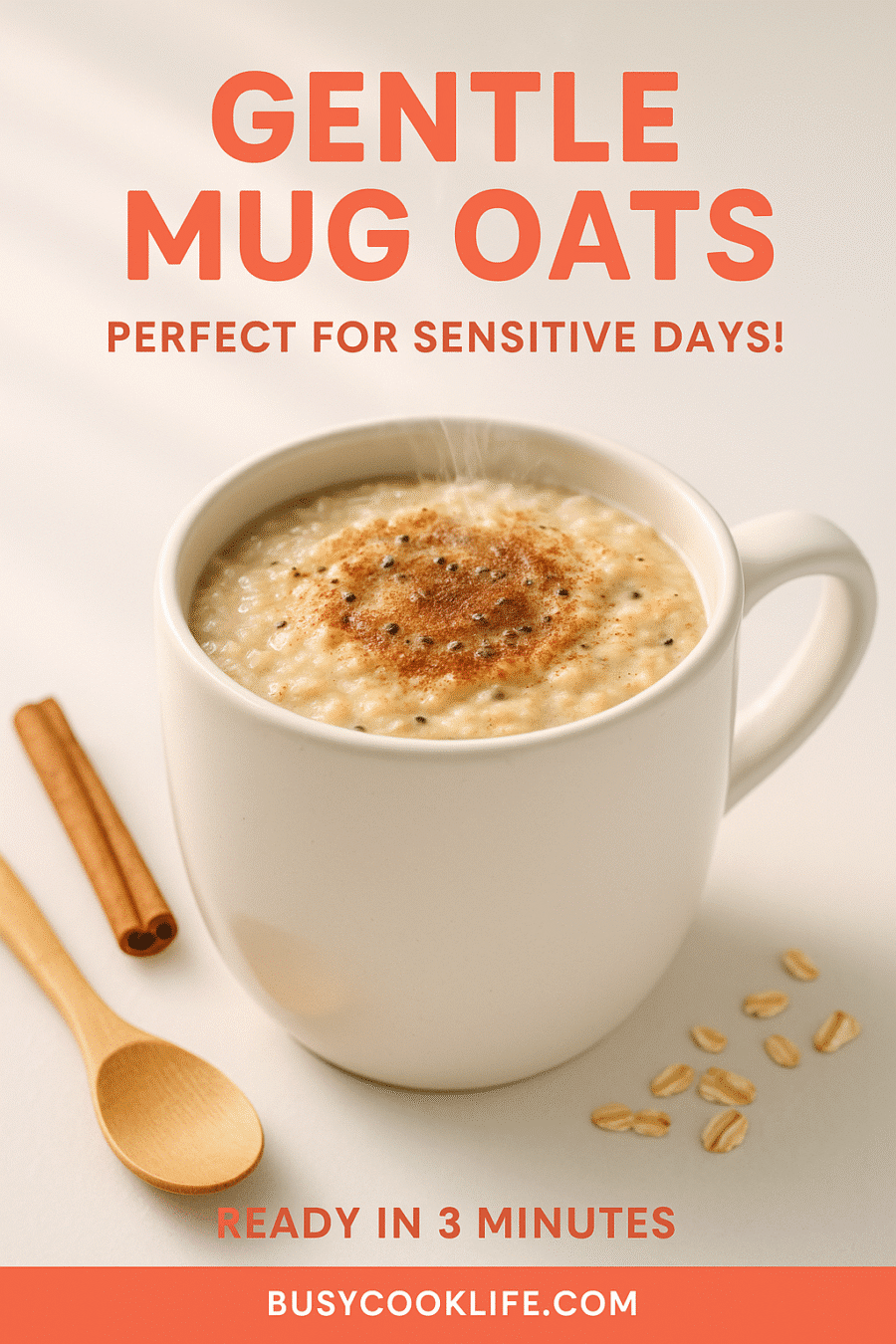
This one’s saved my week more than once: BusyCookLife.com Cozy Mug Oats—microwave oats with milk, cinnamon, and chia for gentle fiber. When I need protein without grease, I rely on the Savory Egg Mug.
- Tiny meals saved me: steady bites meant fewer spikes when the GI tract slowed.
- Bland is beautiful: toast, rice, and bananas calm a sensitive stomach fast.
- Pack snacks: stash gentle food so toddler days don’t force a missed meal and a sugar dip.
“Meal routine beats perfection—cozy basics and steady sips kept me cooking and feeling human.”
For more on avoiding sudden spikes, I tracked trends and read reliable guides on blood sugar spikes.
Real Talk on Side Effects: From Nausea to Low Blood Sugar
Side effects showed up early, and I treated them like kitchen hiccups—small, annoying, fixable. I want honest notes so you can plan, not panic.
Common effects I saw
GI issues came first: nausea, occasional vomiting, and loose stools. Appetite dipped for days at a time. My injection site reddened once or twice.
Low blood sugar risk
When paired with insulin or sulfonylureas, the risk of low blood sugar rose. I kept glucose tablets nearby and told my clinician before any dose change.
What helped me
- Small, bland meals often—toast, rice, bananas.
- Eat more often, lower fat, avoid spicy or fried food.
- Sip clear liquids to stay hydrated; rest when needed.
- Rotate injection spots to protect skin.
Quick note on birth control: pill absorption can dip after starting or after a dose increase. I used backup contraception for four weeks after each start or increase. It felt safer than guessing.
“Most symptoms eased with slow titration, simple food tweaks, and early calls to my clinician.”
| Symptom | What I felt | Home fix | When to call |
|---|---|---|---|
| Nausea / Vomiting | Queasy, low appetite | Bland, low-fat meals; clear fluids | Unable to keep liquids down |
| Low blood sugar | Shaky, sweaty, dizzy | Fast sugar then steady snack | If severe or recurrent |
| Injection site reaction | Redness, tenderness | Rotate spots; cool compress | If swelling or spreading rash |
| Serious pain signs | Sharp belly pain, fever | Stop drug; seek care | Right away—possible pancreatitis |
For a detailed list of possible effects and to learn when to seek help, see this side effects guide.
Results Over Time: Weight Shifts, A1C Wins, and Plateaus
Progress came in inches first, then in numbers—slow, steady, and a little surprising.
In the first months my clothes loosened before the scale moved much. That small change kept me going.
What studies show on weight loss and blood markers
Trials report clear A1C drops and better fasting glucose with regular weekly dosing. Many people saw meaningful changes in body size and blood sugar. In head-to-head studies, this option produced larger reductions than some alternatives.
Why stopping can bring regain—and planning for the long term
I paused once and gained quickly. The research mirrors that. Stopping often leads to regain, while continuing treatment tends to keep gains or improve them.
- My timeline: inches first, then scale, then steady A1C dips.
- Plateaus: normal—tighten sleep, add steps, check meals, and wait another week.
- Maintenance: simple meals, steady walks, same injection day, and patience.
“Judge trends, not days—weeks tell the real story.”
| Measure | Typical change | When it shows | Tip |
|---|---|---|---|
| Clothing fit | Noticeable early | Weeks 4–12 | Use photos, not just scale |
| Scale | Gradual loss | Weeks 8–24 | Track weekly, not daily |
| A1C / fasting glucose | Lower numbers | Months (check at 3 months) | Share readings with clinician |
| Plateau / regain risk | Stalls or rebound if stopped | Can occur anytime | Plan long-term strategy with clinician |
Mounjaro vs. Ozempic vs. Zepbound: Choosing What Fits Your Life
I compared three options the same way I compare pantry staples—what fits my meals and budget?
Quick map: one treats type 2 diabetes, another is approved weight loss with the same active class, and a third treats diabetes while offering heart and kidney benefits for some people.
Where each is approved and how they differ
One product is FDA-approved for type 2 diabetes. Zepbound is tirzepatide approved weight loss. Ozempic treats diabetes and may reduce certain cardiovascular and kidney risks in some folks.
Insurance, access, and practical costs
Coverage matters. Off-label use may not be covered, while an approved weight indication often is. Ask about prior authorization, copays, and manufacturer savings cards before you commit.
Telehealth, prescriptions, and safety checks
Telehealth services like Calibrate or Ro can evaluate you and may send a prescription if appropriate. Always loop in your primary clinician so meds and labs stay coordinated.
- In diabetes trials, tirzepatide produced greater changes in body size than semaglutide in similar groups—still, your goals and side effect profile guide the choice.
- Compare total cost: copays, savings cards, and preferred pharmacies. Ask what speeds approval.
- Be wary of counterfeit pens—use reputable pharmacies and verify packaging.
| Question to ask | Why it matters | How it helps |
|---|---|---|
| Which option fits my medical history? | Safety and benefits vary | Matches goals and lowers risk |
| What dose plan will we try? | Slow titration eases side effects | Keeps nausea down and routine steady |
| Will insurance cover this? | Costs can differ widely | Avoid surprise bills |
If you want real stories about how this worked in day-to-day life, see my weight stories. And if a symptom feels severe, call your clinician right away.
Conclusion
This ended up being less about dramatic change and more about gentle, repeatable steps. I kept a weekly routine, cozy meals, and honest check-ins with my clinician. Small wins mattered more than fast results.
Protect your body: watch side effects early. Ask questions when something shifts. Use a trusted pharmacy for every prescription and report counterfeit concerns to the manufacturer right away.
I’m rooting for steady blood and calmer sugar days. Long-term use can support maintenance, but your care team should guide each step. Breathe, log what helps, and lean on help when you need it—this is a marathon, not a sprint.
FAQ
What is this medication and why did I try it?
I tried tirzepatide because my blood sugar was all over the place and I wanted a practical way to feel better and lose a few stubborn pounds. It combines two gut hormones — GIP and GLP‑1 — to help insulin work after meals and slow stomach emptying, which steadies glucose and often reduces appetite. It’s approved for type 2 treatment; some people use it off‑label for weight management under a doctor’s care.
How does the once‑a‑week dosing work and where did I start?
I started low — a 2.5 mg weekly dose — and my clinician slowly increased it if needed. The idea is slow and steady: raise the dose every few weeks to help your stomach adapt and lower side effects. Typical steps move toward 5–15 mg depending on goals and tolerance.
What common side effects should I expect and how did I handle them?
Nausea, vomiting, diarrhea, and injection‑site reactions were the most common for me. I ate small, bland meals, sipped clear fluids, and timed snacks so I didn’t get too hungry. Those fixes helped a lot. If symptoms were severe or persistent, I called my clinician right away.
Can this cause low blood sugar (hypoglycemia)?
Yes — especially if you’re taking insulin or sulfonylureas. I monitored my glucose more often when doses changed and asked my provider about lowering other meds. If you feel shaky, sweaty, or confused, treat with a fast sugar source and contact your care team.
Are there serious risks I should know about?
There are boxed warnings about thyroid C‑cell tumors in rodents; people with a personal or family history of medullary thyroid carcinoma (MTC) or MEN2 should avoid it. Pancreatitis, gallbladder issues, kidney injury from dehydration, and vision changes are other red flags — seek care if you have severe belly pain, fever, or sudden vision problems.
How do I inject it without making a mess of my life?
Use the pen like a champ — rotate injection sites (thigh, abdomen, upper arm), follow storage instructions, and keep a routine that fits your week. If you miss a dose, take it as soon as you remember within the dosing window or follow your prescriber’s guidance; don’t double up.
What about travel, storage, and avoiding counterfeits?
Keep pens refrigerated until first use, then follow label temps. Use a cooler pack for travel. Buy only from licensed pharmacies and watch packaging for tampering. If something seems off, don’t use it and check with your pharmacy.
How should I eat while my body adjusts?
Small, frequent meals helped me avoid nausea and lows. Hydration mattered — sip water often. Bland choices like toast, rice, or cold yogurt were my go‑tos when my stomach was fussy. Spacing carbs and protein kept my glucose steadier.
Will this affect hormonal contraceptives or other meds?
There’s some note that GI effects could change absorption of oral meds. I used backup or discussed alternatives with my clinician when doses changed. Always review prescriptions with your provider and pharmacist.
What should people with kidney or eye problems know?
Dehydration from vomiting or diarrhea can worsen kidney function, so stay hydrated and call for help if you get very sick. Rapid glucose changes can affect diabetic retinopathy — check in with your eye doctor before and during treatment if you have a history.
How soon do people see weight or A1C changes?
Results vary. Some notice appetite changes and weight shifts in weeks; meaningful A1C drops often appear over months. Stopping can lead to regain, so planning long‑term strategies with your team is wise.
How does this compare with GLP‑1 drugs like semaglutide or with Zepbound?
Each drug has its own approval, dosing, and side‑effect profile. This drug mixes GIP with GLP‑1, which some studies suggest affects weight and glucose differently than GLP‑1 alone. Insurance coverage, cost, and side effects guide the choice — discuss options with your clinician and explore telehealth or savings programs.
Who should avoid this medication right away?
Don’t use it if you have a personal/family history of MTC or MEN2, or if you’ve had a serious allergic reaction to it. Also avoid if you’re pregnant or breastfeeding unless a specialist advises otherwise. Always review your full medical history with your clinician.
What symptoms require emergency care?
Seek immediate help for signs of pancreatitis (severe abdominal pain, radiating to the back), symptoms of a severe allergic reaction (rash, swelling, trouble breathing), or severe dehydration and fainting. If your blood sugar drops very low and doesn’t respond to home treatment, get urgent care.
Can people with type 1 use this?
This medication is not approved for type 1. People with type 1 who are curious should talk to an endocrinologist — using it without clear guidance risks dangerous lows and other complications.

Mounjaro for Diabetes and Weight Loss: My Journey
- Prep Time: 2
- Cook Time: 2
- Total Time: 4
- Yield: 1 serving 1x
- Category: Breakfast
- Method: Microwave
- Cuisine: American
- Diet: Vegetarian
Description
Gentle, nourishing recipes perfect for managing Mounjaro side effects and supporting blood sugar stability. These microwave-friendly options are easy on sensitive stomachs while providing essential nutrients during your health journey.
Ingredients
1/2 cup old-fashioned oats
3/4 cup milk of choice
1 tablespoon chia seeds
1/2 teaspoon ground cinnamon
1 teaspoon honey or maple syrup
Pinch of salt
Optional: 1 tablespoon chopped nuts
Instructions
1. Add oats, chia seeds, cinnamon, and salt to a microwave-safe mug
2. Pour in milk and stir gently to combine
3. Microwave on high for 90 seconds to 2 minutes
4. Stir carefully (mug will be hot) and add sweetener
5. Let cool for 1-2 minutes before eating
6. Top with nuts if desired and enjoy warm
Notes
Perfect for sensitive stomachs during medication adjustment periods. The fiber from oats and chia helps stabilize blood sugar naturally.
PROTEIN VARIATION: Add a scoop of vanilla protein powder for extra nutrition.
MONITOR YOUR BODY: Start with smaller portions if experiencing nausea and gradually increase as tolerated.
PIN THIS RECIPE: Save to your Pinterest boards for easy access during tough days!
FOLLOW BUSYCOOKLIFE: For more gentle, health-supporting recipes that actually work.
Nutrition
- Serving Size: 1
- Calories: 280
- Sugar: 12g
- Sodium: 150mg
- Fat: 8g
- Saturated Fat: 3g
- Unsaturated Fat: 4g
- Trans Fat: 0g
- Carbohydrates: 45g
- Fiber: 8g
- Protein: 12g
- Cholesterol: 15mg